Need, problems and approaches for the artificial construction of tissues using tissue engineering tools.
With the growth of medicine comes the supposed decline of health problems. However, this proportionality doesn’t always hold true. Take organ injury for example. There are currently a few means of treating it: either through medication, surgery, or organ replacement. The former two are meant for minor to slightly major injuries but as it stands currently, high trauma-related acute injuries to any organ require organ replacement. The problem does not end there however as there exist numerous problems with organ replacement. There is a constant lack of donor availability and even if donors do come forward, there is the additional requirement to check for immune compatibility. Hence in recent times, scientists have tried to bypass this inevitable problem by trying to reconstruct their own tissues, in a lab, from scratch. The technical name for such production is de novo synthesis.
They began trying to culture and maintain human cells in 2D culture conditions but quickly found out that a glass plate and a petri dish does not accurately simulate the tissue conditions within an organism. More and more roadblocks began to arise in the issue of simulating tissue environments.
Problems Associated with Tissue Reconstruction
Scientists found it hard to find an artificial construct that effectively imitated tissues for the following reasons:
1) They found it hard to create a construct that could withstand the mechanical stresses that occur to tissue within an organism. The mechanical stresses were not simple perpendicular or modulus stresses that could easily be recreated in a lab. Since an organism was in the constant state of movement, the stress experience was dynamic, anisotropic, nonlinear and viscoelastic.
2) Immune acceptance. If tissue was to be reconstructed, the cells used could either be autologous (from the person who requires organ replacement ), allogeneic ( Different person ) or xenogeneic ( from a different species ). The first option, autologous cells, would not be an issue, but it exists in limited supply. The cells are taken usually stem cells from the bone marrow and they are not in high concentration. The last two options would result in immune incompatibility. However, scientists are using genetic engineering tools to alter the genetic makeup of these cells to inhibit an immune response.
3) Another issue is with the delamination of tissues post-implantation. Let’s say everything goes well and artificial tissue is created in a lab. Once it gets implanted at the site of injury, it needs to successfully reintegrate with surrounding neighbouring tissues and form a strong interconnection with them. Delamination here means forming of layers. The artificial tissue after implantation must have the capacity to form the required laminae or layers to resemble a normal tissue in that particular area of the body.
However, in time scientists created 3D cell cultures grown in special devices that we're able to simulate tissue environments. A few examples of these are:
1) Spinner flasks:
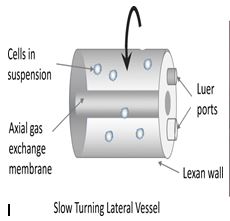
2) Rotating bioreactors: A few examples of these is slow-turning lateral vessel(SLTV) and high aspect ratio vessel(HARV). Both were created by NASA.
The SLTW is cylindrical in shape with an annular space between the two concentric cylinders whereas the HARV is discoid in shape.
Scaffolds
Cells do not exist within a vacuum in the human body or aren’t so densely packed that they form impervious layers. Such layers do exist in nature but are in the minute quantity. In most cases, cells sit in a supporting structure. In the human body, this composes of the extracellular matrix which is a dense mass of connective fibres, collagen, fibroblasts etc, all of which collectively make up the stroma, the supporting structure. Hence, if we are trying to reconstruct a tissue, we need to create a supporting structure known as the scaffold into which cells are seeded during culturing.
Examples:
1) Hyaluronic acid: This is a substance that is generally found in connective tissues and ECM. It has a major part to play in wound healing. In its native form, hyaluronic acid has low mechanical properties making it unsuitable as a scaffold material. However, if certain functional groups are added to it, it can then form chemical cross-links with polymer materials like Poly Ethylene Glycol which will improve its mechanical properties. For example, this was used in a study where Mesenchymal Stem Cells were seeded into a hyaluronic acid sponge. The purpose of this tissue construct was to treat osteochondral defects ( a type of joint defect where there is an injury to both the bone and cartilage ) and the study was successful. The most common means of adding functional groups to Hyaluronic acid is via esterification. This forms Hayff-1, a benzyl ester of Hyaluronic acid. Human Chondrocytes grown on Hayff-1 scaffolds were able to treat chronic cartilage lesions.
2) Alginic acid: It is the main component of seaweed and can be obtained from brown algae. It is a co-polymer containing monomers of Beta-mannuronic acid and alpha-guluronic acid. It has low toxicity, low cost and can easily be chemically modified. Despite such advantageous characteristics, alginate has the drawback of degradation through an uncontrollable and unpredictable process to release divalent ions into its surrounding medium. Covalent cross-linking of alginate gels with different molecules is a useful approach to control this problem. Another drawback of alginate gels in cell-encapsulation studies is the lack of cellular interactions because alginate prevents protein adsorption on itself and therefore it is not able to efficiently interact with the cells. However, modified alginate gels with some proteins, such as lectin, have high cellular binding and interactions and can solve the above-mentioned problem.
3) Poly Ethylene Glycol (PEG): This is a hydrophilic polymer with the formula OH–(CH2CH2O)n–CH2CH2OH. It can be chemically modified to link to and incorporate other biomolecules. An example of this is that PEG hydrogel has been bounded with a peptide of sequence Ala-Pro-Gly-Leu to make them susceptible to enzymes in our body. A major advantage of PEG concerning tissue engineering is that it acts as a good microenvironment for cells to grow in due to its high water content and good mechanical properties. Examples of their use as a scaffold are as follows: a) Photopolymerizable PEG hydrogels are used as a scaffold for chondrocyte, liver cells and muscle cells as it provided in situ gelation using UV light. b) Galactose-functionalised PEG hydrogels were used as a scaffold for hepatocytes. c) Cartilage regeneration was obtained using PEG-chitin-chitosan as the scaffold material.
Approaches to Tissue Reconstruction:
An optimal tissue construct will look like this:
1) It should be an appropriate size and shape.
2) It should have minimal biomechanical function immediately post-implantation and then the function should improve progressively. Imagine constructing a heart that needs time within in vivo conditions before it can start performing its function. That would be a recipe for disaster.
3) It should have the capacity to mature and integrate with surrounding tissues.
4) It should not generate a host immune response.
Here are the basic series of events in tissue engineering: 1) Decide on the tissue to be replaced or treated. 2) Prepare a scaffolding material 2) Obtain primary and subcultures of the cells needed. Cell differentiation may or may not happen at this stage. 3) Seed the cells into the scaffold 4) The cells must adhere and integrate themselves to the scaffold. Cell proliferation and differentiation occur as there is a constant addition of growth factors to the media. 5) Implantation of tissue construct into the body.
However, there are several ways you can do this:
1) The most common approach consists of having a pre-made porous scaffold that is made of either synthetic or natural biomaterials. Once formed, the cells are then seeded into it or on top of it. The scaffold can be made via numerous fabrication technologies. A few are porogen or fiber-based techniques or solid free-form technologies. A disadvantage of this technique is that cell seeding takes a large amount of time and is not efficient.
2) Another approach is to seed the cells during scaffold formation itself. The number of biomaterials that can be used for scaffold formation is limited. Hydrogels of natural or synthetic origin are used as a biomaterial due to their bio-compatibility and mild gelation conditions. Yet at the same time, hydrogels are known for their poor mechanical properties and hence this approach is not usually used, especially when trying to replace a tissue that has a load-bearing function like muscle tissue.
3) A third approach is the decellularization of the Extracellular matrix from the allogeneic xenogeneic tissues. In this approach, we first decellularize the tissue whereby we remove all the cells from it. What remains is the stromal component or supporting tissue structure, which can now act as the scaffold. This "scaffold" is re-seeded with proper cells to create an autologous construct. The cells need not be taken from the patient as well. The main advantages of this technique are that the tissue constructs are biocompatible and the mechanical and functional properties of the construct will closely resemble that of the native tissue. The main disadvantage of this approach is the limited supply of autologous tissues and the immune response generated by non-autologous tissues. Also, there are issues related to the non-uniform distribution of seeded cells and difficulty in removing all immune response generating materials.
4) The final approach involves the use of cell sheets prepared using temperature-responsive culture dishes, a technique known as cell sheet engineering. This technique does not have a scaffold and thus avoids the common problem of scaffold-based approaches which is that as time passes, the scaffold degrades within the body post-implantation. The degraded scaffold is then replaced with autologous ECM, an event that results in fibrosis.
Future Prospects
The ultimate aim of tissue engineering is to bridge the ever-growing gap between organ demand and organ availability. Hence, there is not only a need for it but an urgent need at that. The cells that are used to seed the scaffolds are usually stem cells, a field that is still relatively new. Hence as stem cell research grows, so grows the tissue engineering industry. A challenge in stem cell research is to induce stem cell differentiation into a particular lineage of choice. Recent advancements using gene therapy ( silencing, activation of particular genes) and drug delivery are being used to maintain a particular cell phenotype, a technology that is useful for the aforementioned challenge. The perfect scenario would be the development of immune-transparent stem cells that can differentiate into a target lineage as chosen by the scientist. There still requires study into the combination and interactions between cells and scaffold material to finalize on combinations that will yield the best results. The decellularized approach is one that still remains at the forefront of research due to immune transparency characteristics. However, studies still need to be conducted to ensure that all immune provoking material is removed from the scaffold.
References
1) Hasan, A. (2016). Tissue engineering for artificial organs: Regenerative medicine, smart diagnostics and personalized medicine. Tissue Engineering for Artificial Organs: Regenerative Medicine, Smart Diagnostics and Personalized Medicine, 1–2, 1–717. https://doi.org/10.1002/9783527689934
2) Griffith, L. G., & Naughton, G. (2002). Tissue Engineering--Current Challenges and Expanding Opportunities. Science, 295(5557), 1009–1014. https://doi.org/10.1126/SCIENCE.1069210
3) Lysaght, M. J., & Reyes, J. (2001). The growth of tissue engineering. Tissue Engineering, 7(5), 485–493. https://doi.org/10.1089/107632701753213110
4) Langer, R., & Vacanti, J. P. (1993). Tissue engineering. Science, 260(5110), 920–926. https://doi.org/10.1126/science.8493529
Written By:
Jacob Vacha



Very informative
ReplyDeleteI was diagnose April 17,2015 and find out I'm HIV positive.I was scared because there is no cure for HIV/AIDS but today some people still don't believe that there is cure for HIV, it can only be cured through Africans root and herbs,and our doctor's here in USA few of them know about the African herbal medicine can cure Hiv but they chooses to hide it from us just to make a sales of medical expertise. I did a research online finding way to get rid of my disease,I saw a comment about a herbal doctor on internet Name Dr itua ,who has cured several disease with his powerful herbal medicine, I contacted him on whats-app, chat with him explain my self to him.He said he can cure hiv perfectly well , he gave me his request which i send to him. within 5 days he sent me the herbal medicine through ups courier delivering service And told me how to take the medicine for 2 weeks to get cured,I did for 2 weeks, within this 7 days i notice a very big change in my health and i new some thing great has happened then i went to confirm my result after finishing the herbal medicine for two weeks it was absolutely negative.The doctor who new i was hiv positive was asking me how come i am negative, what did it took to get cure and were did i get this medicine from and how did i get rid of it I told him every thing about the herbal medicine that cure me. imagine doctor telling me not to let anyone know about it,I wasn't shock though i knew they know about the herbal cure but chose to hide it in other to make sales on medicals expertise,if you are HIV positive Or other disease such
ReplyDeleteCancer,Hiv,Herpes,Shingles, Hepatitis B,Liver Inflammatory,Diabetes,Fibroid,Parkinson's,Alzheimer’s disease.contact Dr Itua for any kind of herbal product and remedies through Email Or Website.. drituaherbalcenter@gmail.com www.drituaherbalcenter.com